What is AK ?
It is important to identify and treat these lesions because if left untreated they can develop into invasive squamous cell carcinoma (SCC) which is a type of non-melanoma skin cancer.1, 2
Due to the amount of sun exposure, Australia has one of the highest rates of skin cancer in the world.1
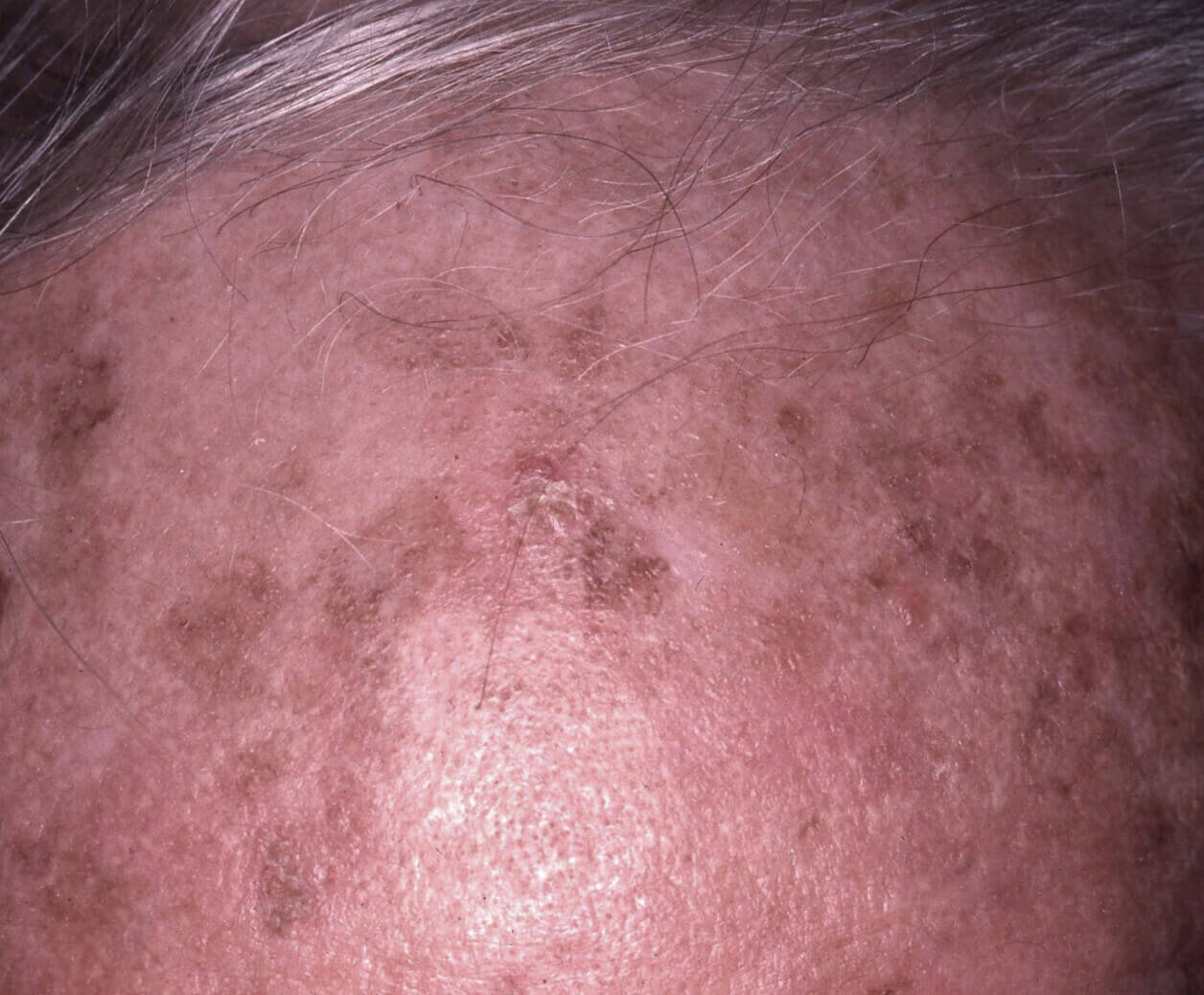
What does Actinic Keratosis look like?
AK can present as a single lesion or a small number of isolated lesions. They may vary in shape and colour.
They can look like small blemishes, scabs or spots that may appear gradually.
They are dry and rough most of the time and often red or brown in colour.
At the more advanced stage, the lesions can become ulcerated and swollen, and begin to bleed or weep.1-4
Is the number of visible AK lesions important? Yes!
There are many reasons why the number of visible lesions is important:
- The presence of multiple AKs indicates that there has been significant ultraviolet (UV) light exposure to that area of the skin.1
- The presence of multiple AKs is an indicator that, in this area of the skin, not only are there multiple visible precancerous lesions, but it is also likely that there are multiple subclinical (eg: non-visible, non-palpable) AK lesions present as well. This area of sun damage is called “field cancerisation”.4,6,7
- The risk of developing cancerous lesions (SCCs that can spread) increases as the number of AK lesions increases. 5
An ultraviolet camera can reveal the extent of sun damage.
AK lesions can regress spontaneously or stay at an early stage, but some of them can evolve into skin cancer in the form of invasive SCC. The biggest concern with SCC is that it can metastasise. Metastatic SCC accounts for about 20% of skin cancer deaths. 1,5
Why Treat AK?
As it is not possible to predict which AK lesion will develop into an invasive SCC, treatment should aim to:4,9
- Reduce the risk of developing an invasive SCC
- Eliminate as many visible and non-visible AK lesions as possible, thus reducing the extent of field cancerisation
- Reduce the rate of AK recurrence
What are the treatments for AK ?
- Lesion-directed therapies which treat individual lesions only1-5
Freezing
This is the technique most widely used by dermatologists to treat isolated AK. Liquid nitrogen is applied directly to the lesion at a temperature of -196°C and forms ice crystals. This kills the cells in the epidermis (keratinocytes) and the lesion falls off the skin
Surgical
therapy
Topical
treatments
There are several options of topical treatments that are applied directly to the lesions.
These treatments can target several lesions at once and can be applied to the whole field cancerisation
Light
therapy
This technique destroys the lesions by applying a photosensitiser which, when activated by light, releases a toxic agent into the AK lesions
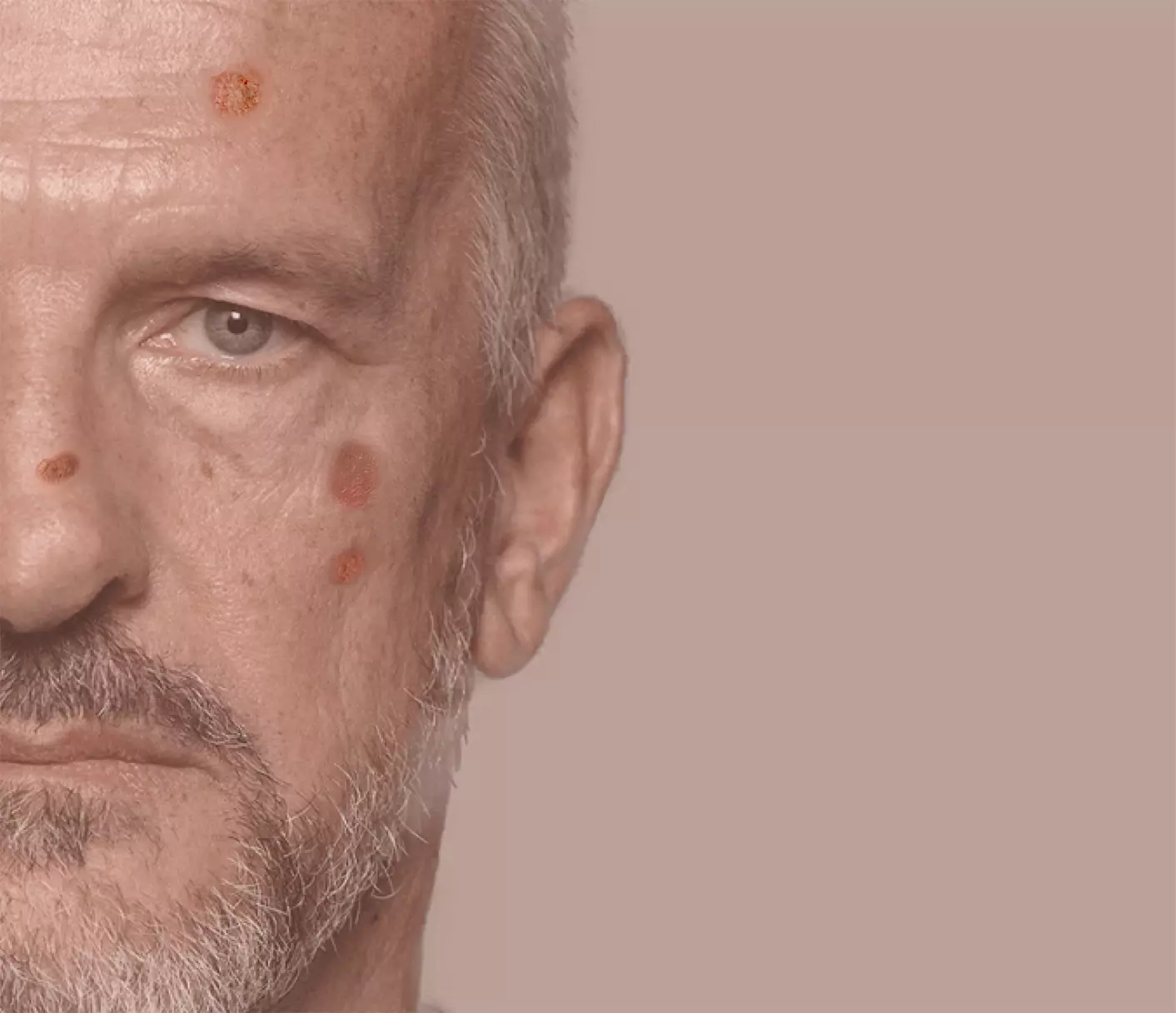
Who is at risk of developing AK ?
The sun’s UV rays are a key factor in causing AKs to develop. In the long term, they can damage the DNA of cells and induce the development of skin cancer.
People who are at higher risk are those who:
Are fair skinned. Fair-skinned people are more likely to be affected because they have less natural protection
Have spent a long time exposed to the sun
Are over 40 (up to 50% of Australians over 40 of caucasian origin will have AK, increasing to up to 80% in the over 60s age group)
Are male (Historically, males tend to spend more time working outdoors - which places them at a higher relative risk of exposure to harmful rays. A balding scalp will also increase sun exposure)
Are taking immunosuppressant therapy
Ways to protect your skin from developing AK
Repeated over-exposure to the sun also speeds up the skin ageing process (premature wrinkles, blemishes, etc.).
Fortunately, there are lots of ways to keep well protected from the sun:11
Limit your exposure to the sun when UV rays are strongest
Wear long sleeves, pants or skirts, a hat, and sunglasses
Apply sunscreen 20 minutes before going out, then every 2 hours, to all exposed areas, not forgetting your ears, hands, and neckline
Use sunscreen with a high sun protection factor that is waterproof
Take care of your skin and if in any doubt, please consult your doctor.
References
- Phan K, Shumack S. Medicine Today. 2021;5:3-9
- Marques E, Chen TM. Actinic keratosis. Treasure Island (FL): StatPearls Publishing. 2021
- Dermatology Expert Group. Therapeutic guidelines 2022;eTG August 2022 edition.
- Stockfleth E. et al J Eur Acad Dermatol Venereol.2017;31 Suppl 2:8-11
- Chia A, et al. Australian Family Physician. 2007;36:539-541
- Willenbrink TJ et al J Am Acad Dermatol. 2020;83:709-717
- Stockfleth E, et al. Curr Ther Res Clin Exp. 2022;96:100661
- Cornejo CM, et al. J Am Acad Dermatol. 2020;83:719-730.
- Stockfleth E, et al. Dermatol Ther (Heidelb). 2022;12:467-479
- Dohil MA. J Drugs Dermatol. 2016;15:1218-1224.
- Sun safety | Cancer Council – Sun safety www.cancer.org.au/cancer-information/causes-and-prevention/sun-safety. Accessed February 2023.